Penalties for hospital readmissions, doled out by the Centers for Medicare and Medicaid Services, are expected to reach about $420 million this year. Faced with ever-increasing fines and penalties as CMS focuses more on care quality than quantity, hospitals must put a plan into place that addresses readmissions to reduce costs and improve patient care and satisfaction.
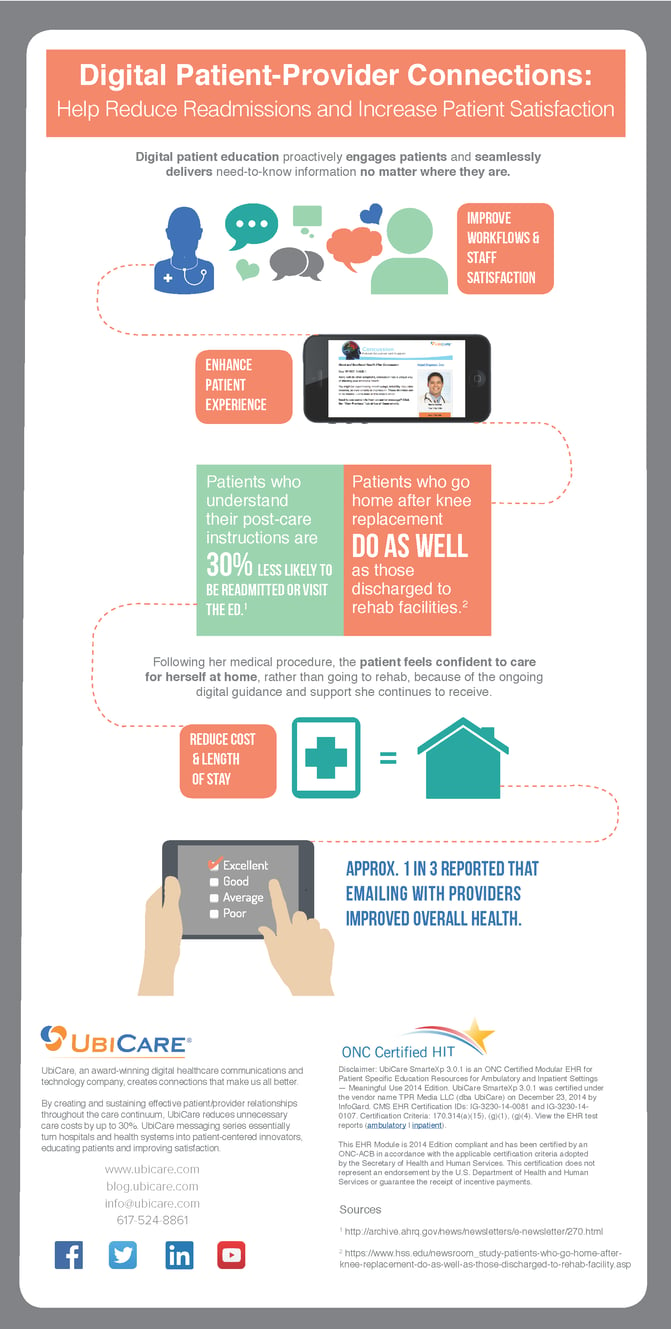
What can hospitals do to meet this goal? Guiding, educating and supporting patient self-managed care can reduce the rate of hospital admissions. Making your patients partners in their care will increase their knowledge and satisfaction—and prevent an avoidable return visit.
In the hospital, patients are in an environment totally focused on providing care. When they leave, they need to feel as if they have that same level of support with them at home. By reaching out to share information that patients need on topics such as follow-up appointments, outpatient services and medication plans, healthcare providers can extend the level of care beyond a hospital’s four walls, making patients partners in their own health, reducing readmissions and, ultimately, improving patient outcomes.
A key measure of success with CMS’s bundled payment plan known as Comprehensive Care for Joint Replacement (CJR) is improving patient outcomes. Under CJR, hospitals must reduce care costs and improve quality of care, not only for a surgery but also through 90 days of rehabilitation and recovery. Patients—and your hospital—do better when you engage patients throughout the entire episode of care and provide them with ongoing timely and actionable education.
Knowledgeable and confident patients are better able to manage their health. As a result, they have better outcomes. And a patient with a good outcome will not end up back in the hospital as a readmission that could have been avoided.
To learn more, read our Case Study: Patient Messaging Linked to Outcomes featured in ORTHOPRENEUR®







