This week, CMS released its final rule for Comprehensive Care for Joint Replacement (CJR), putting 790 hospitals on notice that hip and knee replacement reimbursements from the nation’s largest insurer will be tied to cost containment and high standards for patient care.
Deirdre Wilson

Recent Posts
CMS’s Bundled Payment Plan for Joint Replacement Is Here to Stay
Topics: Improving Patient Outcomes, Comprehensive Care for Joint Replacement
3 Reasons Providers Need to Manage the Entire Episode of Care
Preparing for the CMS Comprehensive Care for Joint Replacement Project
Research continues to find that in-home rehab after joint surgery is as cost-effective and equal in outcomes and patient satisfaction to inpatient rehab facilities.
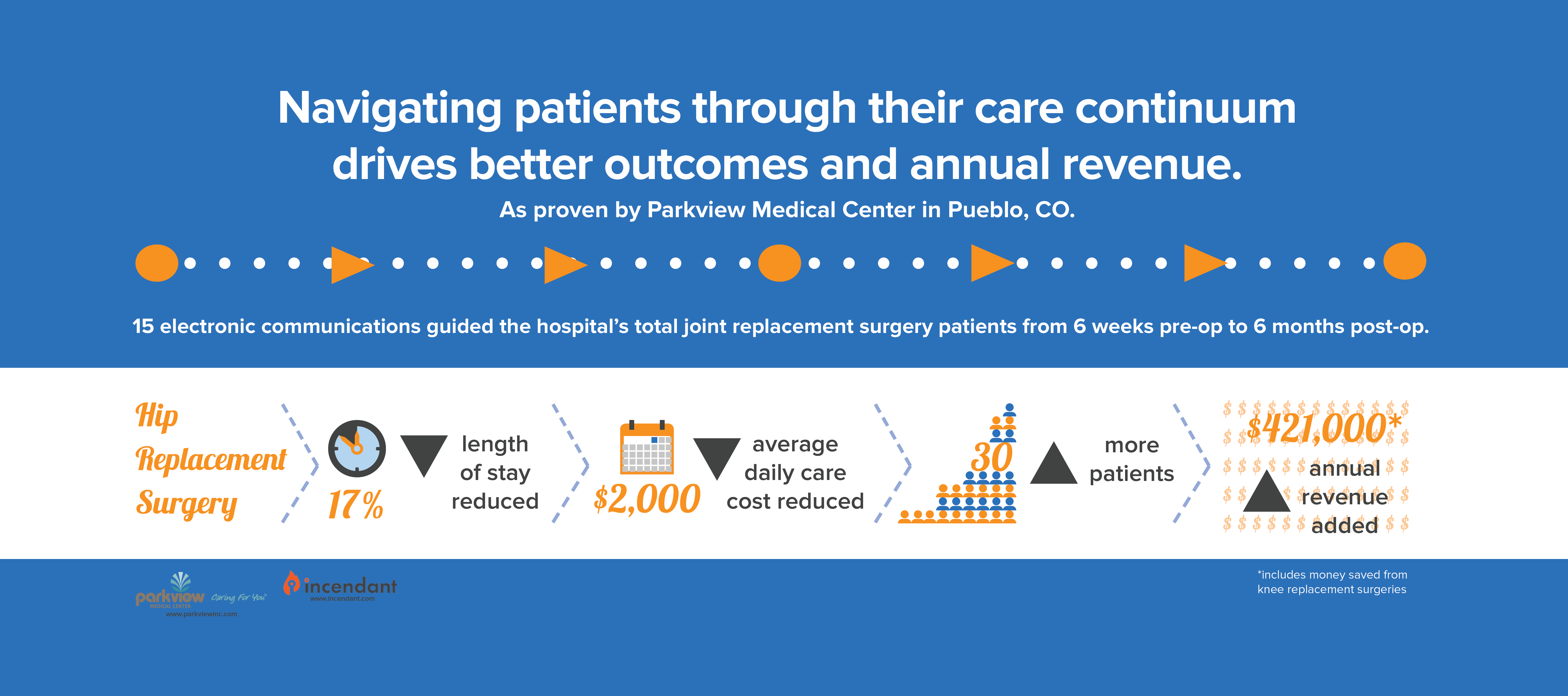
The most important takeaway from the latest CMS effort to rein in costs, achieve positive patient outcomes and lower hospital readmission rates and complication rates is that hospitals must now manage the entire episode of care.
CMS’s Comprehensive Care for Joint Replacement (CJR) bundled-payment program mandates that 790 U.S. hospitals take responsibility for the care quality and total cost of hip and knee replacements, from surgery out through 90 days of rehabilitation and recovery. But the writing is on the wall for all hospitals, health systems and providers: Engaging patients throughout the care continuum—before, during and after surgery—will improve outcomes, decrease readmissions, earn CMS incentive payments and avoid penalties.
Want to Improve Health Outcomes? Start by Building Patient Confidence
You’ve likely heard the adage, “Confidence breeds success.” It’s a saying that doesn’t only apply to goals and achievement. Confidence can also have a powerful influence on your health.
Topics: Meaningful Use, Improving Patient Outcomes, Patient Engagement